
Takeaway: Though insomnia and hypersomnia symptoms may appear to be quite different, both can result in fragmented and low-quality sleep, perhaps due to dysfunction of sleep-wake processes in the brain Effects People with secondary hypersomnia are more likely to experience such symptoms as excessive daytime sleepiness, difficulty waking from sleep, and cognitive dysfunction.
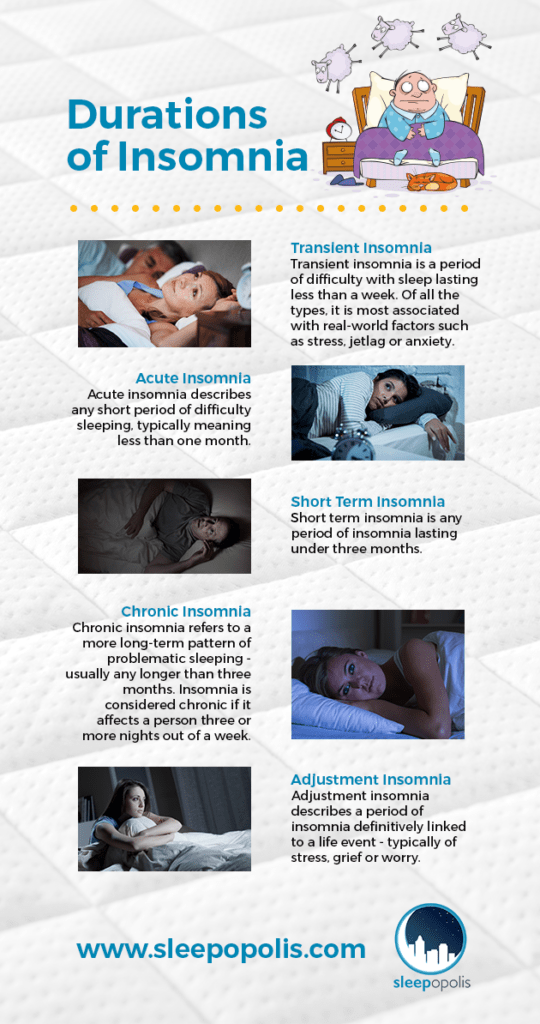
Such symptoms rarely if ever occur with secondary hypersomnia caused by another medical condition or drug side effect. For example, people who suffer from the form of hypersomnia called narcolepsy may experience parasomnias such as sleep paralysis, along with cataplexy, a sudden weakness of the muscles associated with strong emotion and laughter. While the symptoms of insomnia are similar no matter what the cause, hypersomnia symptoms may vary widely depending on the underlying etiology. Fragmented, low-quality sleep may be due to sleep-wake disturbances in the brain in both disorders, and/or hyperarousal of the nervous system in insomnia. Fragmented sleep refers to frequent awakenings that interrupt sleep cycles, leading to less time spent in the deeper, more restorative stages of sleep. Though the symptoms of insomnia and hypersomnia appear to be markedly different, the disorders have a few possible symptoms in common: fragmented and low-quality sleep. Symptoms of secondary hypersomnia, however, typically begin in adulthood, when medical issues and other sleep disorders are most likely to occur.Ĭore symptoms of both primary and secondary hypersomnia include: In contrast to insomnia, which can occur at any time of life from infancy to old age, symptoms of primary hypersomnia most often begin in childhood or adolescence. The inability to sleep even when given the opportunity.Insomnia symptoms typically go away on their own after days or weeks, and do not usually require treatment.Ĭore symptoms of insomnia may occur at any time of life ( 1), and typically include: Though both involve the inability to fall asleep, stay asleep, and/or fall back to sleep, insomnia disorder persists for at least three months, and may not resolve without treatment. Insomnia symptoms are quite common, and differ from insomnia as a chronic disorder. Takeaway: While both insomnia and hypersomnia are common sleep disorders, insomnia is experienced far more often. There are two recognized forms of hypersomnia - primary, or of unknown cause, and secondary, caused by another condition, drug, or sleep disorder. More men than women are affected, in part because more men suffer from sleep apnea, a common cause of hypersomnia. Though not as prevalent as insomnia, hypersomnia is also common, affecting 4-6% of the population. Nearly all of us have experienced an episode of insomnia at some time in our lives, with 33% of the adult population experiencing chronic insomnia. Sleep disorders are found in every country and culture, and the most common of these is insomnia. Insomnia and Hypersomnia: Similarities and Differences

If you feel you may be suffering from any sleep disorder or medical condition, please see your healthcare provider immediately. Note: The content on Sleepopolis is meant to be informative in nature, but it shouldn’t be taken as medical advice, and it shouldn’t take the place of medical advice and supervision from a trained professional. Though the differences might sound straightforward, they are actually quite complex. So what’s the difference between these two sleep disorders? Insomnia means no sleep, while hypersomnia means too much sleep. Stress can worsen the symptoms of both conditions.
Insomnia increases the risk of cognitive dysfunction and accidents, and so does hypersomnia. Both are sleep disorders with a neurological basis, and even share some symptoms and triggers.īoth insomnia and hypersomnia can lead to lost productivity, decreased quality of life, and feelings of fatigue and depression.

Both use the same suffix, which means sleep in Latin. Insomnia and hypersomnia - the words sound similar, and in a few important ways, they are.


 0 kommentar(er)
0 kommentar(er)
